
To view a PDF version of this information, click here.

Diabetes Mellitus is the inability of the body to use and store sugar properly, resulting in high blood sugar levels. Over time, abnormal blood sugar levels alter the biochemistry of the blood and can cause damage to the veins, arteries and capillaries in the body. Small blood vessels are vital to the function of the kidneys, nerves and retina, and these are some of the organs that are affected by diabetes.
Diabetic eye disease is the most common cause of vision loss in the working population, but can affect people of any age. According to population studies, 40-45% of people with diabetes may have diabetic retinopathy. The earliest stages of diabetic eye disease often produce no vision change and may not be detected without a dilated eye examination. These early stages, however, are the best time to intervene-when vision loss can be prevented or minimized in the least potentially damaging way possible. Every diabetic, regardless of age or blood sugar levels, needs to have regular eye examinations to catch this disease in its early stages when the damage may still be reversible. In later stages, some of the damage and vision loss may become permanent.
Gradual damage to the small blood vessels in the retina causes vision loss for several reasons. The vision loss in diabetes is usually painless. Various treatments may be needed depending on the type(s) of damage. These are the 3 most common reasons people with diabetes have vision loss:
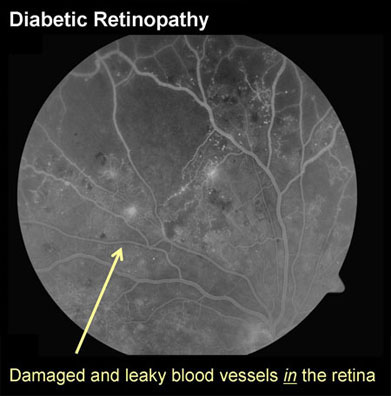
The small damaged blood vessels in the macula (the central part of the retina) can leak fluid and blood. This leakage of fluid can cause swelling and thickening of the macula, a condition known as macular edema. If we think of the eye as a camera and the macula is the film in the camera, then fluid leaking in the macula is like taking a picture with wet, warped film. If leakage persists for a long time, yellowish protein and fat deposits left behind by the fluid can build up inside the retina.
The treatment: The two most common treatments for diabetic macular edema are focal laser and medication injections. Laser is used to target the damaged, leaking blood vessels and stop the leakage. Injections of molecular medications into the eye are also used to stop fluid leakage from damaged blood vessels. Sometimes these two types of treatment are used together, and sometimes repeat treatment sessions are needed.
When blood vessel damage from diabetes is more severe, the retina tries to compensate by growing new blood vessels. This is the retina's natural response to poor blood flow. Unfortunately, rather than helping the situation, these new blood vessels make things worse because they are abnormal and fragile and they rupture and bleed very easily.
If they continue to grow, abnormal blood vessels in the eye can bleed into the vitreous cavity causing severe floaters and profound vision loss. Also, if not treated, abnormal blood vessels can become larger and then turn into scar tissue which tightens and contracts over time. Because they are still attached to the retina, these scarred abnormal blood vessels can pull on the retina and detach it from the back of the eye, potentially causing severe and permanent loss of vision.
The treatment: The best time to treat abnormal blood vessel growth is before bleeding occurs. Panretinal laser is applied to the peripheral retina where the blood flow is the poorest. This slows the growth of new abnormal blood vessels and usually causes existing abnormal blood vessels to shrink and wither away. Multiple sessions of laser are usually required to control this more severe form of diabetic retinopathy.
If there is severe bleeding inside the eye, then laser treatment cannot be performed because the blood blocks the doctor's view into the eye, making it unsafe to use laser. If this happens, waiting and keeping the head elevated at all times often helps the loose blood in the eye settle down enough to enable the doctor to apply laser on a future visit. If this blood does not settle down or clear after a month or more, then vitrectomy surgery may be needed to clean the blood out and restore vision.
In very severe cases, abnormal blood vessels causing a retinal detachment may have to be peeled off the retina using vitrectomy surgery and then the retinal detachment can be repaired.
Sometimes, the blood vessel damage is so severe that there is not enough blood flow to nourish the macula, the central part of the retina. The macula gradually becomes starved for nutrients and oxygen and is not able to function well, resulting in vision loss. Unfortunately, the blood vessels of the macula are too tiny to be repaired and if this problem occurs it cannot be reversed. But even if the blood flow is not adequate, treating the other problems above can still maximize what vision there is in the eye, and tight blood sugar control can help minimize further loss of blood flow.
It is important that your blood sugar be consistently controlled for several days prior to seeing your ophthalmologist for an exam. Uneven blood sugar causes a change in your eye's focusing power, interfering with your ophthalmologist's measurements.
Although blood sugar levels may vary from hour to hour, a blood test known as the hemoglobin A1C level, can measure the general trend of your blood sugar levels over a few months. Your primary care doctor will check your hemoglobin A1C level, and when you visit Valley Retina Associates, our staff and doctors will routinely ask about your hemoglobin A1C level so that your retina doctor can provide the best care for your eyes.
In addition to blood sugar levels, it is also important to have good control of your blood pressure and cholesterol levels as high blood pressure and high cholesterol can cause greater retina damage in diabetics.
Diabetes is a complex disease that affects the entire body. The patient, the retina doctor, the general ophthalmologist, and the primary care doctor are all part of a team, with the goal of keeping the patient's eyes and body healthy. Your Los Angeles retina doctor will work together with your other doctors to coordinate your care. We recognize that the most important part of your care, and the most difficult, is the patient's part: diet, exercise and control of blood sugar levels.

